
We tend to know how to respond when someone has a cast for a broken bone, or even a Band-Aid on a small wound. We show compassion and let them know we hope they feel better soon. But what about the wounds, the traumas and the healing that are related to our mental health?
Despite all the progress that has been made, our culture still perpetuates mental health stigma. This can have serious implications for those seeking help, as well as those helping others in need. We know mental health is as important as physical health, so let’s look at ways to remove the barriers that come with mental health stigma.
What is mental health stigma?
Mental health stigma is seeing someone as “other” based on what we know about their mental health. Mental health stigma involves judgment and shame toward mental health struggles and the act of seeking help. Sometimes we might place the stigma on ourselves.
Mental health stigma is a result of our need to differentiate and categorize, to stereotype in order to make sense of the world and maybe to create a false sense of safety. But the problem with trying to simplify any one person’s mental health journey is that we each experience the highs and lows of living our unique lives.
Let’s remember that everyone is fighting a battle and deserves our compassion, and that means even ourselves. The curious thing about mental health is that it is unique to each individual and we are all navigating a constant flux, even if we aren’t aware of it.

Why is mental health stigma harmful?
The term “stigma” has its origins from ancient Greek and was historically synonymous with branding criminals and enslaved people. This matters because we unconsciously mark mental health in the negative even by using the word “stigma.” We would do best to, in the words of the late Matthew Perry, “...make stigmas a stigma.”
Mental health stigma creates all kinds of obstacles for those seeking help, for those looking to support them and for the rest of society. When someone is considering improving their mental health but they hear others say things like “you don’t need help, you just need to toughen up” or “what’s wrong with you?” – there is much less chance they will seek help.
Sometimes these voices aren’t outside but make their way into our own patterns of thinking, holding us back from getting the help we deserve.
Where does mental health stigma show up?
Mental health stigma shows up in our local communities. At work. Even among the people we love.
Different cultures attach stigma to mental health in different ways. In cultures where individuals are expected to “be tough” and “keep on moving,” it can be hard to even consider seeking help. Stigma shows up in communities where support tends to be lacking and everyone is expected to take care of themselves and leave others alone. Ironically, the toughest person may very well be the one who goes against the norm and sets out to improve their mental health.
For example, first responders are some of the people most susceptible to mental health stigma (more on that here). Not only do individual cultural influences keep first responders from seeking mental health treatment, but EMS and law enforcement cultures also tend to create obstacles. Yet, the enormous amount of trauma with which these individuals come into contact on the job makes their mental health a top priority.
Employers are slowly taking steps to normalize mental health in the workplace, but this approach is only a few years in the making.
Quite a few years ago, I recall becoming aware that I was in need of counseling while at a company conference as I listened to a speaker talk about his mental health struggles in the context of his job. Even though I’d grown up familiar with recovery and therapy approaches due to my own family dynamics, I had never sought counseling on my own.
But facing an adult decision of seeking therapy instantly stirred up thoughts of “less than” and “what will people think of me?” and “will this affect my job?”
When my supervisor, who was also a good friend, asked how I felt about the conference, I initially hesitated to say much because I feared being stigmatized for my own mental health needs. When I responded that I thought my biggest takeaway was that I need counseling, I waited anxiously for his response. He was already reaching into his desk to write a number on a piece of paper while saying, “I know someone you might resonate with. He’s helped me a lot.” I received the response we all hope for but rarely get – compassion and real, supportive solutions.
My own stigmatization of mental health almost got in the way of getting the help I needed. Fortunately, in this instance, stigma did not show up in my local community or work. While this is not most people’s experience when seeking help, it should be.
Recognizing our own biases
What role do we as individuals play in perpetuating mental health stigma? How are we adding to negative perceptions of those struggling with depression, disordered eating, anxiety, obsessive-compulsive disorder and other mental health issues? Or are we celebrating, supporting and compassionately engaging mental health?
We may not be aware of our bias when it comes to mental health. Just like prejudices around race, ethnicity or gender, we likely grew up around certain attitudes about mental health – for ourselves and others. One of the simplest approaches to checking your bias is to ask if you are marginalizing yourself or others in how you think.
Questions to ask ourselves about our mental health bias include the following:
- When I’m struggling, do I see myself as “less than”?
- Do I perceive someone else who is struggling as “other,” not like me?
- How do I think about someone seeking therapy?
- Do I offer a sense of safety for anyone seeking to improve their mental health?
More than recognizing our biases, we need to move toward a more inclusive, supportive paradigm for mental health care. As noted earlier, everyone (including ourselves) is fighting a battle that others know nothing about. Getting to know the individuals we consider “other” quickly dissolves the biases.
How does mental health stigma prevent access to support?
There are several ways that stigma impacts people seeking treatment. Landry Weatherston-Yarborough, LPC, CEDS-S, NCC, executive director at Eating Recovery Center and Pathlight Mood & Anxiety Center, names three ways stigma can prevent access to support:
- Stigma reduces the likelihood that people will be honest about what they are experiencing for fear of being judged.
- Stigma can be internalized so that people judge themselves for experiencing mental health difficulties. This often results in their not reaching out for help.
- Stigma also prevents professionals from screening for or ruling out some diagnoses based on stereotypes or personal beliefs. The lack of an accurate diagnosis can be a major barrier to effective treatment.
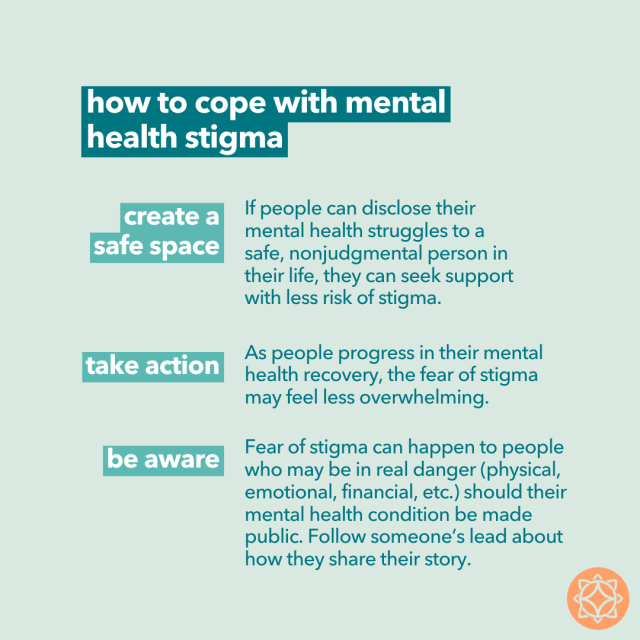
Tips to cope with mental health stigma
When it comes to coping with mental health stigma, we ourselves can take the first step toward change. Consider these tips for working through our fear of stigma in order to get (and give) help as needed:
- Create a safe space. If people can disclose their mental health struggles to a safe, nonjudgmental person in their life, they can seek support with less risk of stigma.
- Take action. As people progress in their mental health recovery, the fear of stigma may feel less overwhelming.
- Be aware. Fear of stigma can happen to people who may be in real danger (physical, emotional, financial, etc.) should their mental health condition be made public. Follow someone’s lead about how they share their story.
It is possible to be the catalyst for destigmatizing mental health within our own family, our social circles, even our communities. When we share our personal experiences of mental health stigma or the positive outcome of seeking care, we can turn the tide and change perspectives.
“I think that it's valuable for people – who are willing and in a position to safely do so – to share their stories of lived experience with stigmatized situations to normalize and personalize these experiences,” shares Weatherston-Yarborough.
When we own and share our own experience, we open the door for others to feel seen or heard – and reduce the power of fear and stigma.
Real stories from our community
What does that look like? At Pathlight, we have helped many people take steps against mental health stigma to get the care they need. Here we find out what it means to them:
“Mental health stigma is people telling me that because of my mental health issues, I won’t be successful. My way of coping with that is by doing the opposite and proving them wrong! That has helped me to just keep going. I want to fight against all odds.” – Maddy, Pathlight alum
“I used to be ashamed of telling people about the mental health issues I face. Once I realized that my mental health does not define me, I was able to recognize my worth. If someone can't accept a part of me, it is their loss. I can surround myself with people who accept me for who I am.” Gloria, Pathlight alum
Weatherston-Yarborough shared that another alum she worked with was raised in a culture that held a lot of stigma around mental health treatment. The alum’s family had been fairly negative about her enrollment in treatment, though they were willing to be involved. They engaged in family therapy and Pathlight’s family education opportunities, and were able to significantly decrease their sense of stigma once they saw how helpful treatment was for their child.
If you’re struggling with your mental health and want to connect with others who understand what you’re going through, Pathlight offers a variety of free support groups open to you and your family.
Need more support? Call us at 877-825-8584 to speak with a mental health professional and get matched with the exact support you need.


